A glimpse into our research
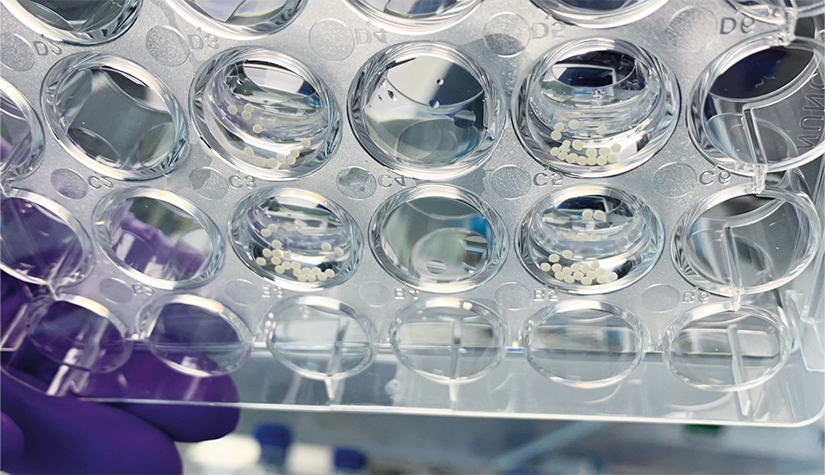
Our research goal is to develop complex human in vitro models that recapitulate as much as possible the human brain in both healthy and disease states. We are fascinated by the human brain, particularly its complex functionality and interplay with other organs. Our aim is to develop an in vitro human brain model with which we are able to recapitulate different aspects of human physiology and their relating pathologies. Specifically, we currently focus our attention on Parkinson`s disease (PD), a neuropathological disease that on the one hand is becoming an increasing burden for our society whilst on the other hand, it can serve as a representative model for other, less studied neurodegenerative diseases. Our work is based on the usage and further refinement of human brain organoid and assembloid technology.